Dr. Jennifer Pena, a Puerto Rican native and proud U.S. Army veteran, considers stigma a familiar foe. As a member of the Army’s Latinx community for over a decade, she not only experienced stigma firsthand but also saw how it impacted her patients. Hispanic communities in general often face this stigma. “When I came out of the military, I had never taken care of an HIV patient,” says Dr. Pena. “That wasn’t due to a lack of wanting to serve that population. There are just not many HIV patients in the military. And a lot of those in the veteran population just didn’t feel comfortable seeking treatment for HIV.”
During her long battle with stigma, Dr. Pena has found creative ways to overcome and educate. She describes herself as a patient and provider. “I try to view everything from the lens of both ‘what if I was a patient, what would I need to know?’ And also as a provider, giving the most culturally appropriate, comprehensive information I can,” Dr. Pena mused.
Her expertise is especially influential on initiatives at Q Care Plus, child company of Avita Care Solutions, and providers’ communication with Hispanic communities and Latinx patients.
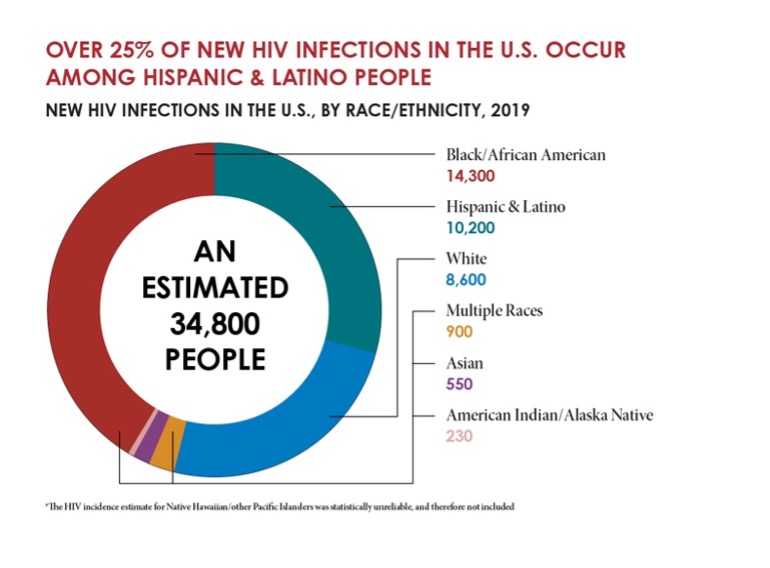
Serving the Hispanic/Latinx community is vital to reaching zero new HIV infections, for which the Centers for Disease Control and Prevention (CDC) has set a goal to reach zero by 2030.
According to AIDSvu, recent data suggests “there were only…6 Hispanic/Latinx PrEP users for each new HIV diagnosis” within that racial group. This is compared to 26 white PrEP users for each new HIV diagnosis among white people.
Additionally, Hispanic/Latinx people represented 27% of new HIV diagnoses and 17% of PrEP users.
What accounts for this disparity? And, more importantly, how can the medical community and teams at organizations like Q Care Plus support people from all backgrounds to reach health goals?
Cultural Barriers for Hispanic Communities
Dr. Jennifer Pena, MD, FACP, says, “Culturally most Latin American communities have a huge stigma with anything that’s sexual health or reproductive health in general. Hispanic cultures tend to be heavily Catholic and Christian. Which are not always supportive of the most comprehensive sexual health education.”
According to the National Health Institute, “HIV-related stigma serves as a determinant of health among” Latinx communities. This includes negative attitudes and beliefs directed at people living with HIV.
According to the CDC, for some Hispanic and Latinx communities “social and structural issues such as xenophobia, language barriers, poverty, mistrust of the health care system, and limited access to high-quality health care” impact the ability to access HIV prevention and treatment. In turn, this continues to drive the infection rate for new HIV cases within the Hispanic/Latinx community.
Shawn Smith, 340B Senior Account Executive at Avita Care Solutions believes that community involvement and education goes a long way in respecting culture and reducing any barriers of entry to care that might be related to culture.
“We are involved with a lot of the events throughout the year to celebrate Hispanic culture and establish that we are trying to drive change in all communities through inclusive care,” says Shawn. “With one of our partners, which holds an annual Hispanic Food Bazaar, for example, that showcases Hispanic food and culture. We partner with our organizations in South Florida to celebrate Latino Gay Pride, otherwise known as Gay Ocho. And that’s just a couple of examples of our annual efforts to support our partners. Being involved on the ground and showing up for the communities we serve is at the core of who we are as an organization.”
Avita Care Solutions team members recognize that they are continuously learning about a variety of cultures. But, “Just listening to the communities we serve through strategic partnerships with these community organizations and then tailoring our services to that really sets us apart from big box pharmacies,” says Shawn. “Their service offerings are more generalized whereas we can really develop those key relationships in the community and tailor our messaging as needed.”
It Starts with Language
Dr. Pena by no means thinks breaking down stigma is easy. She does, however, know where to begin.
“It starts with having conversations. We must talk about health issues like HIV, PrEP, condoms, and more to see a change in our communities. What we do successfully at Q Care Plus that other organizations struggle with is reaching the Spanish-speaking audience with their native language.”
From something as simple as a medical handout, to Q Care Plus’s Spanish version of our website, to hiring native Spanish-speaking staff—the medical team has truly thought of it all under Dr. Pena’s leadership.
“Our medical team cannot assume that people are bilingual, and they read English,” says Dr. Pena. “And, even if they do, reading medical language in your second language is not easy. You really need to put medical information in their primary language. And using Google Translate isn’t going to cut it. It may be accurate, but it lacks nuance. One of my projects since I started at Q Care Plus has been to review and edit all the written information our providers used to communicate with patients. I’ve been adding the colloquial flavor of the Spanish language, if you will, making it more readable for our patients. We do this because we care. Tailoring the language to that community says a lot. Q Care Plus is going above and beyond to create a welcoming healthcare environment for Spanish speakers.”
Avita Care Solutions as a whole works diligently to ensure that patients who are Spanish speakers are able to receive quality care in their language. Shawn says, “In communities like South Florida and South Texas, we make sure our pharmacists are all bilingual and almost all the staff in those locations speak Spanish. The ability to adapt is what sets us apart. We work with translators to make sure any physical materials we pass out in our pharmacy locations are tailored to specific communities.”
Historical Hispanic and Latinx Mistrust in the Medical System
Latinx/Hispanic communities historically have a lack of trust in the medical system due to years of discrimination.
Dr. Pena says, “The issues with the trials and studies that were done here in Puerto Rico with birth control and the mass sterilization that was done on women here and in New York still carries a lot of weight with Hispanic and Latinx Populations. It still causes mistrust.”
Dr. Pena is referring to birth control pill trials conducted in Puerto Rico in 1955. Because it was a U.S. territory, scientists John Rock and Gregory Pincus saw an opportunity to conduct medical trials for less cost in lower socio-economic Puerto Rican communities. Ignoring public health ethics and potential side effects from previous trials, Rock and Pincus offered women housing options in exchange for participation in the trials. Women in these trials were subjected to a variety of side effects, poor standards of care, high dosages of hormones, and a lack of transparency on the long-term health impacts of the birth control pill. The trials were later scrutinized for colonialism, deceit, and exploitation. But the damage was already done.
Because of this and other historical trials “There’s still a lot of mistrust. Messaging matters. And making sure our materials and attitudes are culturally competent to reduce the bias goes a long way,” says Dr. Pena.
Immigration Status
For patients who are undocumented, accessing care is nearly impossible outside of a telehealth environment.
In a recent study on HIV stigma in the Latinx community, one 45-year-old male participant mentioned, “Many people won’t go and seek out services because they are afraid it will affect their immigration status…for fear of being found out as undocumented individuals, they don’t seek help.”
Q Care Plus is proud to serve undocumented patients. “A lot of people that are coming here who might not be documented might feel like they can’t get clinical care,” says Dr. Pena. “But we can provide them that care. We want them to feel safe and at ease. They will never be judged for their documentation status, and our services are completely confidential and discreet to make this possible.
Meeting people where they are at with health literacy is key. “You have to be able to reach patients at a community level. Because, otherwise, remember, they’re living in a situation where they’re trying to stay away from the public light,” says Dr. Pena.
Q Care Plus partners with community organizations across the country in some of the country’s most vulnerable communities to reach people at that community level.
Are you ready to get started on PrEP or learn about other services provided by our team? Visit Avita Care Solutions to learn about how we can be your partner in care.

Dr. Jennifer Pena is aboard-certified, internal medicine and former US Army and White House physician with over 15 years of clinical experience. She has expertise in executive medicine, digital and telehealth, and clinical leadership. Her extensive experience in providing high quality, patient-centered and comprehensive primary care/hospital care/telemedicine, and in leading and collaborating with multidisciplinary teams to improve world-wide access to healthcare makes her an asset to the quality care the Avita Care Solutions team provides.
In addition, Dr. Pena was a featured speaker and medical contributor for several TV and radio networks, and at various national, international, and virtual conferences on digital and telehealth, COVID-19 and Veteran’s affairs.

Shawn Smith holds a Bachelor’s in Business Administration and Management from the University of Kansas. He has almost a decade of experience working at pharmaceutical and healthcare companies. His focus is on strategic account management and reimbursement management. At Avita Care Solutions, Shawn is responsible for the promotion of Avita Specialty Pharmacy and 340B services. These are targeted to physicians, nurses, discharge planners, and case managers with complex disease states.
